

Can innovations in robotics, visualization, and digital intelligence advance the delivery and quality of care? Can future tech enable better outcomes for surgeons and their patients and long-term value for healthcare providers? These are big questions that are complex and pivotal as healthcare systems around the world work to address staffing challenges, rising costs, and global health issues.
At Intuitive, we see a future of care that is increasingly technology-enabled and digitally informed. We believe there’s tremendous potential to harness current and future innovations in robotics, artificial intelligence (AI), machine learning (ML), and advanced visualization to address stressors facing surgeons, physicians, care teams, and the institutions where they practice.
While there is no panacea, no magic bullet to solve systemic healthcare issues, there are innovations available from Intuitive today, and inflight for the future, that have potential to drive meaningful change, particularly in robotic surgery. These range from how data insights may enhance technology training for surgical residents and fellows, to how technology can be thoughtfully used to augment surgeons’ capabilities. And they include the continued integration of digital intelligence into robotic surgical systems and instruments. This is a development that began more than 25 years ago when Intuitive put computer technology, what became known as the da Vinci standard system, between a surgeon and a patient.
Our goal two decades ago, today, and well into the future is to enhance surgeon capabilities, support informed, real-time decision making, and help advance the possibility of ever more positive and reproducible patient outcomes for surgeons and care providers.
“See one, do one, teach one.” This has been the fundamental approach to surgical education for millennia. While this apprentice-based approach continues to hold tremendous value, it is also highly dependent upon student access to informed instruction. The availability of experienced surgeons to share their knowledge can impact the time it takes for new surgeons to hone their skills—and the variability among educators can make it hard to prescribe detailed and objective training measures.
At Intuitive, we seek to complement the “see one, do one, teach one” philosophy through our cloud-based learning content, remote case proctoring, simulation tools, and advancements in pre-operative planning. This evolved approach could help increase the number of surgeons trained to use robotic systems for minimally invasive procedures and expand access to robotic surgery for patients globally.
Engineers, data science experts, and medical professionals at Intuitive are thinking past current technology and exploring new ways to analyze data drawn from robotic surgical procedures performed by highly experienced surgeons. After two decades of usage data and more than 10 million procedures performed with da Vinci systems, Intuitive teams are using AI/ML technologies to provide insights that may help surgeons using robotics learn not only from cases of lower complexity, but also from more complex cases that address anomalies and complications. This is all to help reduce the impact of surgical variability and deliver better, more consistent outcomes.

Today, Intuitive’s immersive vision experience is integrated into the da Vinci surgical system. Years of research and development, as well as advancements in optics and imaging processing technologies have made it possible for surgeons using da Vinci systems to experience a highly magnified 3DHD view of the surgical site with true depth perception. This means they can see tissue planes clearly, identify structures, and stay oriented in the anatomy.1 To further enhance surgeons’ visual acuity, Intuitive developed Firefly—a near-infrared fluorescence capability—that helps surgeons visualize vessels, the bile duct, and tissue perfusion.1
The impact of these technologies has spurred additional investments in the exploration of new imaging and fluorescent imaging agents. Teams at Intuitive are working to provide more data, reduce visual noise, and help surgeons see well beyond what’s possible with the naked eye. By exploring fluorescent agents that can target critical anatomy or abnormal tissue, such as the ureter or prostate cancer, Intuitive teams aspire to help surgeons enhance surgical outcomes by reducing injury to important structures and to give surgeons enhanced visualization that helps enable surgeons to perform complex procedures with greater assurance.
The future of robotic surgery will feature increasingly intelligent tools and devices designed to augment, inform, and extend surgeon and care team capabilities. Stapling in robotic surgery is just one such innovation.
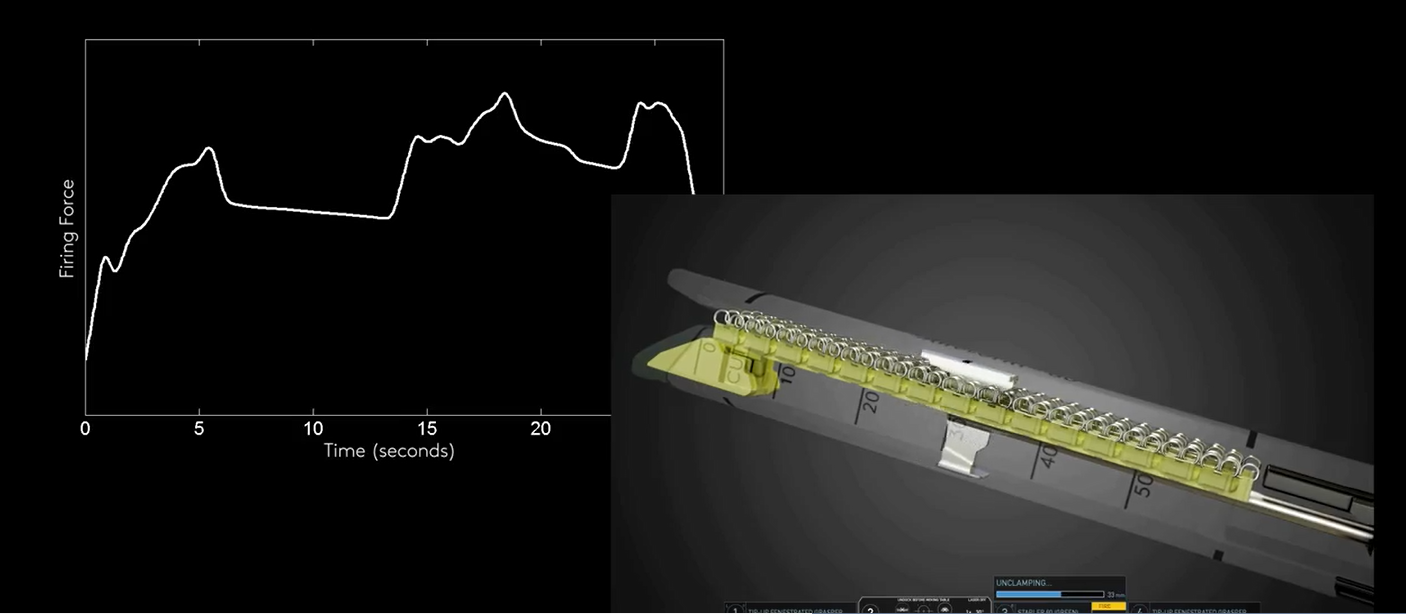
Stapling has long been used in surgery when removing parts of an organ, when cutting through and sealing tissues, or when creating connections between structures. One of the requisites for an effective staple line is to ensure the correct amount of tissue is being compressed between the staple jaws before firing the stapler. Skilled surgeons learn the art and science of stapling through hands-on experience across multiple cases and procedure types.
But what if a stapler had built-in intelligence that could assess tissue thickness in real time? That is exactly the challenge Intuitive engineers addressed in the development of the company’s latest stapler family. Intuitive teams integrated intelligence into its SureForm staplers to help ensure more consistent and optimally formed staples. With 1,000-plus measurements per second, SureForm staplers make automatic adjustments to the firing process as staples are being formed and as the transection is being made to help optimize a consistent staple line and prevent tissue damage across a range of tissue thicknesses.1
Now, imagine if Intuitive leveraged that same marriage of advanced hardware, software, and digital intelligence to enhance surgeon senses. Intuitive is currently exploring new technology advancements to do just that, including augmenting sensory information while the surgeon is using da Vinci instruments. Advancements like this will become more pervasive in future offerings to help care teams drive consistent, reproducible outcomes.
With the rapid pace of advancement in robotic technology, data collection, and the ability to provide real-time feedback to surgeons, what is considered “standard of care” for specific procedures continues to evolve and advance. Prostatectomies are a great case in point.
In the 20 years since robotic-assisted surgical (RAS) approaches were introduced for prostatectomies, RAS has become the standard of care in the United States,1 where previously they were predominantly performed through open surgery. The steady transition from an invasive, open procedure to a minimally invasive robotic procedure speaks to the clinical impact possible when advanced technology is put in action by skilled surgeons and care teams.
Get a sneak peek at the future of da Vinci vision. Complete the form below to see how the latest fluorescent imaging agent under development may help identify cancerous tissue during a prostatectomy using a da Vinci system.2
Thank you for your submission.
Important safety information
Patients should talk to their doctor to decide if surgery with a da Vinci system is right for them. Patients and doctors should review all available information on nonsurgical and surgical options and associated risks in order to make an informed decision.
Serious complications may occur in any surgery, including surgery with a da Vinci system, up to and including death. Serious risks include, but are not limited to, injury to tissues and organs and conversion to other surgical techniques which could result in a longer operative time and/or increased complications.
For important safety information, including surgical risks and considerations, please also refer to www.intuitive.com/safety. For a product’s intended use and/or indications for use, risks, full cautions and warnings, please refer to the associated User Manual(s).
Individuals’ outcomes may depend on a number of factors, including but not limited to patient characteristics, disease characteristics, and/or surgeon experience.